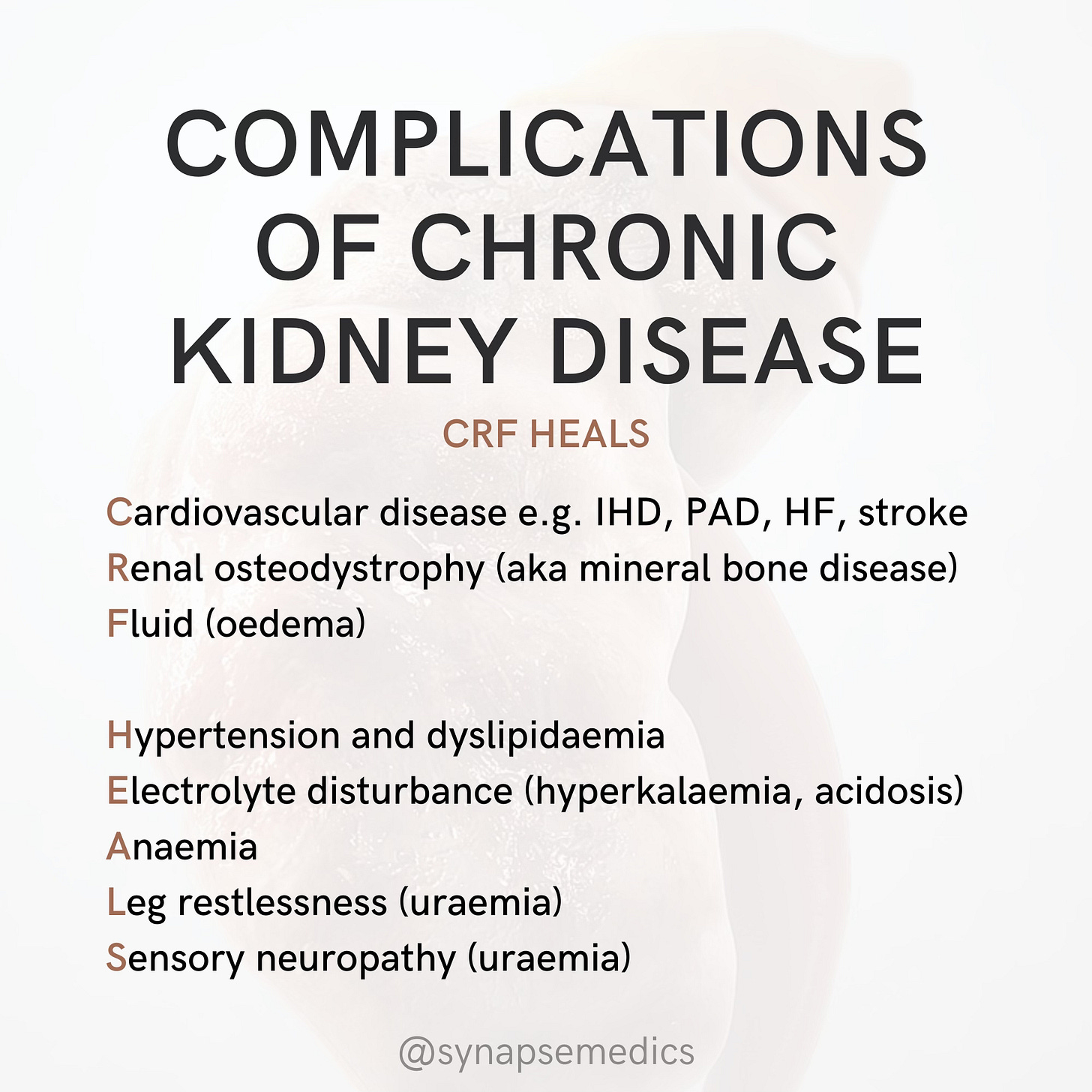
Complications of Chronic Kidney Disease
Mnemonic of the week: Complications of CKD
Condition of the week: Chronic Kidney Disease (CKD)
Definition
Progressive condition resulting in the gradual loss of kidney function over months to years
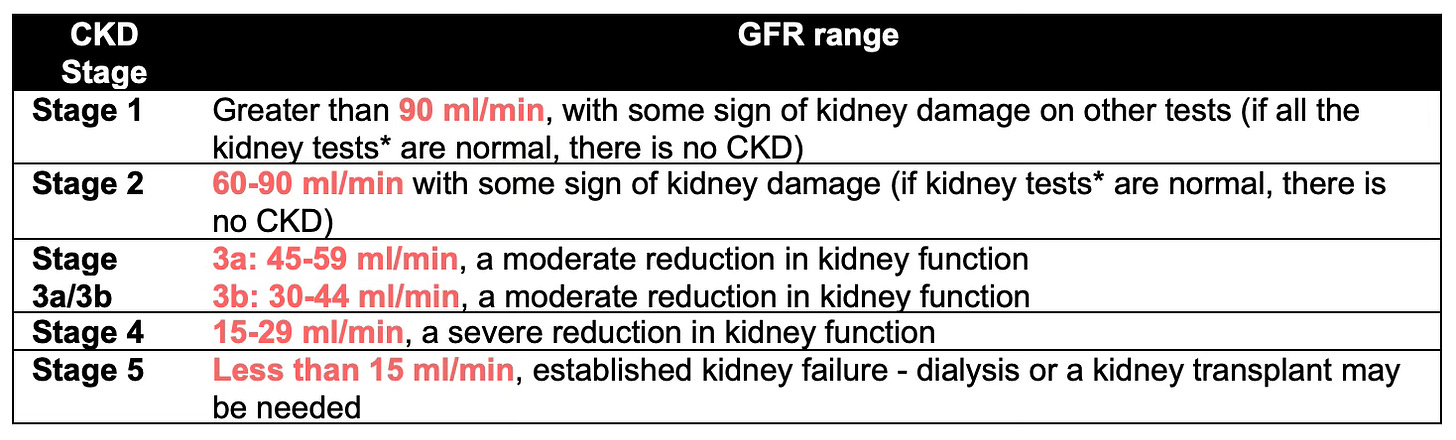
Defined as abnormal kidney function for over three months, with either reduced glomerular filtration rate (GFR) or markers of kidney damage
Classified into 5 stages based on the level of kidney function (stage 1 is the mildest and stage 5 is the most severe)
Patients with CKD are at increased risk of developing complications such as cardiovascular disease, anaemia, and bone disease.
Most commonly caused by hypertension or diabetes mellitus
Clinical features
Usually asymptomatic initially (and generally diagnosed following abnormal urea and electrolyte results)
Late-stage disease may become symptomatic. Symptoms may include:
Oedema e.g. ankle swelling, weight gain
Polyuria
Lethargy
Pruritis (secondary to uraemia)
Anorexia (may result in weight loss)
Insomnia
Nausea and vomiting
Hypertension
It is helpful to think about the functions of the kidney and how an impairment of each function can manifest:
Investigations
Urine: dipstick (haematuria ± proteinuria), microscopy, culture and sensitivities (to exclude infection), protein or albumin to creatinine ratio on first-pass morning urine specimen
Bloods: FBC (renal anaemia), U&Es (electrolyte imbalances, raised creatinine), LFTs, HbA1c, bone profile, bicarbonate, BNP (raised)
eGFR: <60ml/min/1.73m2
Renal ultrasound: measures size and excludes calculi/obstruction
Management
Stage 1-4 without uraemia:
1st line ACEi/ARB e.g. lisinopril 2.5-5mg (consider dapaglliflozin + statin)
2nd line CCB
Stage 5: dialysis (via AV fistula) > kidney transplant
Managing complications:
HTN: aim for <140/90 and ACR<70 (or PCR <100) - lower BM, higher ACR/PCR in diabetes
Proteinuria: ACEi/ARBs
Anaemia: IV Fe/EPO if Hb <100g/l
CKD-mineral bone disease: restrict phosphate intake, phosphate binders e.g. sevelamer, activated vitamin D
Fluid and salt restriction
Acid base status: oral sodium bicarb (aim for bicarb >22)
Hyperparathyroidism: cinecalcet